If you’re injured on the job in Ohio, one of your first concerns will be medical treatment, especially if the injury is severe and you’ll be away from the workplace for a while. The cost of hospital stays, surgeries, doctor visits, and rehabilitative sessions adds up fast, and without some type of coverage, you’re going to be in a tough financial situation. No one could blame you for wondering, “Does workers’ comp pay medical bills?”

The best aspect of Ohio’s workers’ compensation system is that if your treatment is approved, you pay nothing out of pocket: no copays, no deductibles. This coverage applies to injured workers whose employers participate in the Ohio Bureau of Workers’ Compensation (BWC) state fund, as well as those working for self-insured employers.
While the goal is the same in both systems, the way medical bills are handled can vary. In either case, you’ll need to follow state law to make sure your care is approved and your bills are paid. This blog explains how the workers’ comp system works when it comes to medical coverage and how a workers’ compensation lawyer can protect your right to payment.
How Workers’ Compensation Covers Medical Bills in Ohio
In Ohio, your medical bills are paid differently depending on how your employer is insured. If your employer is insured through the state system, the BWC reviews your claim and, if it’s approved, pays your medical providers directly. This means that your healthcare providers send their bills to the BWC rather than to you, so you don’t have to arrange payment yourself.
If your employer is self-insured, they handle these responsibilities without going through the BWC’s billing system. The employer or their third-party administrator reviews treatment requests, approves them if they meet Ohio’s workers’ comp standards, and pays the provider directly. In both systems, you will not be charged for covered treatment as long as it’s related to an allowed condition and you follow the approval requirements.
Reporting your injury as soon as possible is critical in either case. For state-fund claims, this means filing a First Report of Injury (FROI) with the BWC. For self-insured employers, you must notify your employer immediately so they can begin reviewing your claim.
Prompt reporting helps get your treatment authorized more quickly, reduces the risk of payment delays, and makes it harder for the insurer or employer to argue the injury happened somewhere else or that the treatment was for an unrelated condition. Because the process is detailed and any mistakes can affect your benefits, it’s important to have a skilled workers’ compensation attorney guiding you from start to finish.
Types of Medical Expenses Covered
In Ohio, workers’ compensation will usually cover medical care tied to an allowed condition in your claim. Examples of these conditions include:
- Traumatic injuries suffered during work-related duties, such as a fall, crush injury, or burn;
- Occupational illnesses that develop over time as a result of workplace conditions. Examples include respiratory diseases from exposure to dust or chemicals, or repetitive stress injuries like carpal tunnel syndrome;
- Aggravation of pre-existing conditions, provided the work injury or occupational disease substantially worsens the condition.
If your injury or illness is linked to that condition and the care is medically necessary, it’s usually eligible for payment. While BWC state-fund and self-insured employers use different systems to review and pay for care, the scope of what’s covered is largely the same.
Emergency Care
If you suffer work-related injuries, workers’ compensation covers the ambulance ride, emergency room treatment, and any related emergency procedures. In these situations, you have the right to choose where you go for emergency care and who provides it. Once your condition is stable, follow-up care must come from a BWC-certified provider, and you must get approval before receiving most non-emergency treatment. This approval process helps ensure your care is covered under the workers’ compensation system.
Hospital Stays and Surgeries
When your work-related injury requires inpatient hospitalization, overnight stays, or outpatient surgery, workers’ compensation pays for the facility fees, the surgeon’s fees, and any necessary anesthesia services. This coverage includes pre-surgical testing and post-surgical follow-up visits. In both state-fund and self-insured claims, non-emergency surgeries need prior authorization to confirm they’re necessary and related to the allowed condition.
Physician and Specialist Visits
Workers’ compensation covers doctor’s visits as well as referrals to specialists like orthopedic surgeons, neurologists, or occupational medicine doctors. With state-fund claims, these providers must be BWC-certified; in self-insured claims, they must be on the employer’s approved list. This coverage for injured workers includes initial assessments, follow-up visits, treatment planning, and progress evaluations.
Diagnostic Testing
Tests such as X-rays, MRIs, CT scans, and lab work are paid for when they’re used to diagnose or monitor your condition. Many of these tests require pre-approval so the payer can confirm they’re necessary for your treatment. If a test reveals another injury or illness unrelated to your claim, workers’ compensation won’t cover treatment for that unrelated issue.
Prescription Medications
Drugs prescribed to treat your allowed condition are generally covered. If your claim is state-funded, you typically fill these prescriptions through a pharmacy that participates in the BWC’s network. Self-insured employers may have their own pharmacy arrangements, but still limit payment to medications they’ve approved for your claim. Coverage includes refills, but you may need periodic reviews to confirm the medication is still necessary.
Rehabilitation Costs
Physical therapy, occupational therapy, and other forms of rehabilitation are frequently needed to regain movement, strength, or function after an injury. Workers’ comp pays for these services when they’re prescribed by your treating provider and approved in advance. Ohio guidelines sometimes limit the number of sessions allowed, though additional sessions can be approved if your provider shows they’re medically necessary for recovery.
Special Medical Equipment and Supplies
If you need ambulatory devices such as crutches, braces, wheelchairs, or supportive footwear, workers’ compensation can pay for these items. In most cases, they must be approved before purchase. This category can also include supplies like dressings or splints when they’re prescribed for your allowed condition. For more expensive equipment, the payer may require quotes from multiple suppliers before giving approval.
What Ohio Workers’ Compensation Will Not Cover
Ohio workers’ comp pays only for treatment connected to the allowed conditions in your claim. Even if you believe a service relates to your injury, the BWC or your self-insured employer won’t pay unless it meets Ohio’s medical necessity rules and fits within the scope of your approved conditions. Knowing what’s excluded helps you avoid surprise bills.
- Non-Work-Related Injuries or Illnesses: Workers’ compensation won’t pay for treatment that isn’t linked to work-related duties. For example, you might injure your back in a fall at work. Weeks later, your medical provider diagnoses a knee injury from the same fall. You can request to add the knee injury as an allowed condition, but you must prove it’s related to that workplace incident. If the knee problem came from another cause, it can’t be added and won’t be covered.
- Unapproved or Unauthorized Treatment: You must get approval before most non-emergency care. In both state-fund and self-insured claims, you need to use BWC-certified providers after emergency care. While you may choose any hospital or provider for immediate emergency treatment, ongoing care must be delivered by a provider certified through the Ohio Bureau of Workers’ Compensation. If you get treatment without following those rules, the payer can deny the bill even if the service is for an allowed condition.
- Treatment Outside Medical Necessity Guidelines: Ohio applies medical necessity standards to decide if a service should be paid for. If the provider for an injured worker recommends care that falls outside those standards, the payer can deny it. Your provider can request an exception, but they must justify the service and get approval before you receive it.
Can You Choose Your Doctor?
In Ohio, injured workers have the right to choose the doctor who treats them, but the choice must meet certain guidelines. For both state-fund and self-insured claims, you must use a BWC-certified provider once your emergency care is complete. This certification ensures the provider can bill the BWC directly and follow its treatment approval rules. If you see a non-certified provider for ongoing care, the BWC can refuse to pay the bills.
You can change your treating doctor if you believe another provider would better manage your recovery, but you must follow the change process for your claim type. In a state-fund claim, you file a C-23 form with the BWC to make the switch. In a self-insured claim, you contact your employer or TPA for approval. Following these steps ensures the new doctor’s services are authorized and the bills are paid.
Denial of a Medical Bill? Here’s What to Do
A medical bill can be denied in an Ohio workers’ comp claim for several reasons. The payer may decide the treatment isn’t linked to an allowed condition, the provider wasn’t approved, or the care wasn’t authorized in advance. Understanding the reason for the denial helps you determine how to address the problem.
Your first step should be to contact your attorney. Depending on the type of employer, the appeal process differs:
- In state-fund claims, your attorney will appeal the Managed Care Organization’s (MCO) denial or a BWC order, and have it set for a hearing before a District Hearing Officer (DHO).
- In self-insured claims, your attorney will file a motion, which is then scheduled for a hearing before a DHO.
Sometimes denials result from paperwork errors that a provider can correct and resubmit, but if the payer still refuses to cover the bill, you’ll need legal guidance. An attorney ensures the right motions are filed, deadlines are met, and your case is presented properly before the Industrial Commission of Ohio.
Speak to an Ohio Workers’ Compensation Attorney Today
In Ohio, workers’ comp can pay your medical bills if the treatment is connected to an allowed condition in your claim. The system works differently for BWC state-fund and self-insured employers, but both require you to follow their approval rules, use the right providers, and act quickly after an injury or diagnosis of an occupational illness.
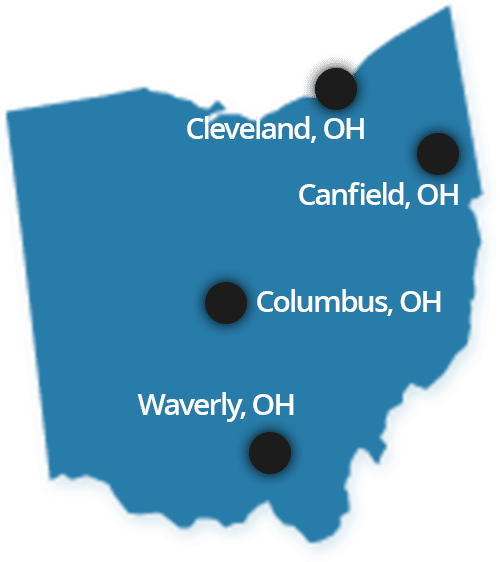
You should always speak with a lawyer about your claim to make sure you’re getting the full coverage you’re entitled to. At Plevin & Gallucci, we have been representing workers like you for more than 50 years. Our workers’ compensation lawyers can review your claim and medical records, help you file your claim, challenge improper denials, and help you secure the medical treatment you need. To schedule a free consultation with our legal team, call us today at 1 (855) 4-PLEVIN or send us a message online.
Related:
- Does Workers’ Compensation Pay for Pain and Suffering?
- Ohio Workers’ Compensation Lump Sum Settlements
- When To Get a Lawyer for a Work Accident Injury
- Do I Have to Use Sick Leave or Vacation for My Work Injury?
- Workers’ Compensation Settlement for Back Injury
- Can You Refuse Surgery Under Workers’ Compensation?
- Can I Be Fired for Filing a Workers’ Comp Claim in Ohio?
- What If I Was Injured While Working Off-Site or Traveling for Work?
- Ohio Workers’ Compensation Appeals Lawyers